Patient Info
Dental Implants
Cosmetic Dentistry
General Dentistry
When it comes to permanent tooth replacement, dental implants are an excellent choice. But how long do dental implants last? The factors that contribute to the longevity of dental implants depend largely on the lifestyle and overall oral hygiene maintained by the patient. In the last several years, dental implant technology has progressed to such an extent that implant failures resulting from rejection or malfunctions have essentially disappeared from the past. Preexisting medical conditions, diseases, and implant misuse are more likely factors that cause an implant to fail.
Generally, a dental implant intends to remain a permanent fixture in your mouth. Trusted sources report a success rate of 90 to 95 percent for dental implants over 10 years.
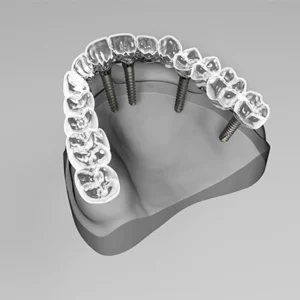
A dental implant procedure replaces the missing teeth. It consists of a titanium post, which is placed into the jawbone under the gum line surgically. It acts as an artificial tooth root, providing a sturdy foundation for dental crowns and tooth replacement. These tooth implants look, feel, and function like natural teeth, restoring the smile's appearance and functionality.
To understand the question, "How long do dental implants last?" let's outline the three main components of a dental implant:
The exposed abutment and crown are typically more prone to damage than the implant itself.
When adequately maintained with proper brushing and flossing, the implant can endure a lifetime, provided the patient undergoes regular dental check-ups twice a year. However, a crown typically lasts around 10 to 15 years before regular wear necessitates replacement, although exceptional dental care could prolong its lifespan beyond 15 years.
Moreover, the location within the mouth influences the expected durability of a dental implant. Implants positioned at the back of the mouth endure more pressure from chewing, potentially leading to quicker failure compared to implants situated near the front of the mouth.

Here are some simple steps you can take to help dental implants last longer:
Mini dental implants are mini versions of traditional dental implants. They're often used in situations where there's not enough space or bone density for regular implants. These mini-implants consist of a titanium post that's inserted into the jawbone to support crowns or dentures.
As for how long they last, it's essential to note that mini dental implants have a slightly different lifespan compared to standard implants. While traditional implants can last a lifetime with proper care, mini dental implants typically have a shorter lifespan, usually ranging from 5 to 10 years.
However, their longevity can vary based on factors like oral hygiene, bone density, and overall health. Regular dental check-ups and maintenance can help increase the lifespan of mini dental implants.
So, if you're considering mini dental implants, it's essential to discuss their longevity and maintenance with your dentist to ensure they're the right option for you.
Dental implants are a good option for many people, but they're not suitable for everyone. Generally, individuals with good overall health, adequate bone density in their jaw, and healthy gums are good candidates for dental implants.
However, certain factors may affect eligibility for dental implants, such as:
Consult with a dentist or oral surgeon to find out if dental implants are the right option for you. They can assess your oral health, discuss treatment options, and assist you in making an informed decision about restoring your smile with dental implants.
"How Long Do Dental Implants Last?" is a question many individuals ponder when considering dental restoration options. With proper maintenance and regular dental check-ups, it can last a lifetime, offering a durable and natural-looking solution for missing teeth.
It's crucial to prioritize oral hygiene and follow the recommendations provided by your dentist to ensure the longevity of your dental implants. By taking proactive steps to care for your implants, you can enjoy the benefits of a healthy and confident smile for years to come.
Ready to explore the possibilities of dental implants? Springhill Dental Health Center, located on Springhill Ave, AL, is here to help. Whether you're a new patient or seeking expert dental care, you can schedule an appointment today. New patients can call (251) 265-7808 while existing patients can reach us at (251) 343-1521. Let's embark on the journey to restore your smile and enhance your dental health together!
With proper care and maintenance, your implants should last a lifetime. Regular dental check-ups and adhering to recommended oral care routines can help maximize the lifespan of dental implants.
Yes, dental implants can fail, although it's not very common. The failure can occur for various reasons, such as infection, bone loss, peri-implantitis, implant overload, poor osteointegration, etc.
Dental implants can last about 25 years with proper care, surpassing the average lifespan of bridges and dentures, which is around 10 years.
Tooth loss can significantly impact your ability to eat and speak normally. Fortunately, restorative dentistry offers solutions like implants, bridges, or dentures to replace missing teeth. Among these options, dental implants emerge as a permanent, convenient solution that closely resembles natural teeth. But what is the Success Rate of Dental Implants?
However, deciding on dental implant surgery entails careful consideration due to the upfront cost and lengthy treatment process. Understanding the success rate of dental implants becomes crucial in making informed decisions about oral health treatments.
In this blog, we delve into the factors influencing the success rate of dental implants, providing valuable insights into their reliability and effectiveness. Join us as we explore the world of dental implants and uncover the keys to their success.
The average dental implant success rate is around 94% after 15 years. However, specific factors contribute to the dental implant success rate, including implant diameter and length, periodontal health, general health, and the patient's age.
Several factors play an important role in determining the success rate of dental implants, ranging from the type of implant utilized to its placement location. When engaging in discussions regarding dental implant surgery and success rates with your dentist, it's important to consider the following:
The diameter of the implant post significantly impacts overall success rates. Studies indicate that dental implants with a smaller post diameter (<3mm) are more prone to failure, whereas those with a larger post diameter (>4mm) tend to have higher success rates.
The quality of the bone where the dental implant is positioned is another critical determinant of success rates. Research indicates that implants installed in denser, higher-quality bone are less susceptible to failure compared to those placed in softer, lower-quality bone.
A recent 2022 study examining mini implants revealed a correlation between bone quality, quantity percentage, and maximum insertion torque value (ITV). Essentially, higher bone quality translates to increased stability, as the ITV indicates.

Shorter implants tend to exhibit higher long-term success rates compared to longer ones. Following dental implant surgery and osseointegration, there is typically minor marginal bone loss. A study conducted in 2018 revealed that implants shorter than 7mm experienced less average bone loss, thus offering enhanced long-term stability and reducing the likelihood of late implant failure.
Older patients are at a greater risk of experiencing implant failure compared to younger individuals. Research from 2005 indicates that patients aged between 60 and 79 years have a notably higher risk of implant failure. This risk can be attributed to the likelihood of older patients having other health conditions that may impede the healing process, such as uncontrolled diabetes, blood disorders, and head or neck cancers.
The success of dental implants often depends on their location within the mouth. Implants positioned in the front of the mouth have higher success rates than those placed in the back. Front teeth are subjected to less pressure than rear teeth, which experience more intense bite force. Consequently, restorations in the back of the mouth may wear down more quickly, and implant posts may become loose.
A study revealed that dental implants located at the rear of the lower jaw had a failure rate of 3.3%, whereas those in the front of the upper jaw had a lower failure rate of just 1%.
Dental implants offer a lasting solution for individuals seeking to preserve their natural smile despite missing teeth.
These implants are titanium posts that oral surgeons surgically position in the upper or lower jaw, serving as robust anchors for replacement teeth. The procedure, conducted in-office, boasts a remarkably high success rate.
The titanium tooth root implant is strategically placed to fuse with the jawbone, a process known as osseointegration, which typically spans several months. During this period, temporary teeth are used until the bone and implant bond securely, forming a sturdy foundation for the new teeth.
Following a span of four to six months, your dentist can affix the posts to the implants, completing the permanent restoration of your smile.
Some benefits of dental implants include:
Dental implant surgery primarily involves two techniques: endosteal and subperiosteal implants. Endosteal implants, the standard type, are surgically implanted into the jawbone. Subperiosteal implants, on the other hand, are placed beneath the gum tissue directly on top of the jawbone.
Endosteal implants typically exhibit a higher success rate compared to subperiosteal implants. With a direct embedding into the jawbone, endosteal implants boast a success rate of 95%. In contrast, subperiosteal implants offer less structural stability and have a slightly lower success rate of 93% after 5 years.
So, what is the success rate of Dental Implants? Understanding the success rate of dental implants is essential for individuals considering tooth replacement options. Through exploring various factors that contribute to implant success, we've gained valuable insights into the reliability and effectiveness of this restorative procedure. With proper care and consideration, dental implants offer a long-term solution for restoring smiles and enhancing oral health.
Ready to explore dental implant options and enhance your oral health? Contact Springhill Dental Health Center on Springhill Ave, AL, to schedule an appointment. Whether you're a new patient or seeking expert dental care, contact us at (251) 265-7808 for new patients or (251) 343-1521 for existing patients. Let's embark on the journey to restore your smile together!
The success rate of dental implants varies depending on the type utilized. Among the options, the endosteal implant, the most prevalent type, boasts a success rate of approximately 95%.
Older patients and those with underlying health conditions may face a higher risk of dental implant failure. Factors like uncontrolled diabetes, blood disorders, and certain cancers can impede the healing process and affect the long-term success of dental implants.
Patients play a vital role in implant success by adhering to post-surgery care instructions. This includes maintaining good oral hygiene, attending regular dental check-ups, and promptly addressing any concerns or discomfort with their dentist.
Ever wondered, "Can a rotten tooth make you sick?" It's not just about avoiding toothaches; it's about your overall health. Tooth decay turning into a rotten tooth brings risks beyond your teeth—infections affecting your entire body. Your body often hints when it's not doing well, and your teeth play a role.
Taking care of your teeth connects to your immune system and your overall well-being. Regular dental checkups and simple oral care habits go a long way.
The integral role of dental health in overall well-being highlights how the condition of your teeth and gums can significantly impact your general health. Here's why dental health is crucial for your overall well-being:
Poor oral health is linked to various health problems, including heart disease, diabetes, and respiratory issues. Maintaining good dental health helps reduce the risk of these conditions.
Healthy teeth enable proper chewing, which is essential for effective digestion. Dental problems can lead to difficulties in eating, impacting your nutritional intake and overall health.
A healthy smile contributes to self-esteem and confidence. Dental issues, such as rotten teeth, can affect your appearance and, subsequently, your mental well-being.
Dental infections, if left untreated, can spread to other parts of the body, leading to systemic infections. Regular dental care helps prevent these infections.
Dental problems, especially those affecting the front teeth, can impact speech. Maintaining good dental health ensures clear and effective communication.
Oral bacteria from dental infections can be aspirated into the lungs, contributing to respiratory problems. Good dental hygiene helps maintain respiratory health.
As you age, dental health becomes even more critical. Proper oral care can prevent issues like tooth loss, gum disease, and other dental problems associated with aging.
Here are some strategies for preventing tooth decay and ensuring timely dental care:

Schedule bi-annual dental checkups to monitor oral health. Professional cleanings help remove plaque and detect early signs of decay.
Brush teeth twice daily using fluoride toothpaste. Floss daily to remove plaque between teeth and along the gumline.
Consume a diet rich in fruits, vegetables, and dairy products. Limit sugary and acidic foods that contribute to tooth decay.
Consider professional fluoride treatments to strengthen tooth enamel. Use fluoride toothpaste for added protection against decay.
Dental sealants are protective coatings applied to molars to prevent decay. These are especially beneficial for children prone to cavities.
Frequent snacking exposes teeth to acids and sugars. Opt for healthy snacks and limit between-meal snacking.
Tobacco contributes to gum disease and tooth decay. Quitting smoking supports overall oral and systemic health.
Implementing these strategies fosters a proactive approach to dental health, preventing decay and promoting overall well-being.
A tooth abscess is a severe condition resulting from untreated dental issues. Delve into what constitutes a tooth abscess, its symptoms, and its impact on overall health. Prevention is the key to avoiding this serious dental concern.
Here are some signs that a tooth infection might be spreading to the rest of your body:
- Fever
- Swelling
- Pain
- Bad Breath
- Bitter Taste
- General Malaise
- Difficulty Breathing or Swallowing
- Headache
- Earache
- Gastrointestinal Distress
If you notice any of these symptoms, it's crucial to seek prompt dental care. Dental infections can escalate, affecting not only your oral health but also your overall well-being. Early intervention helps prevent complications and ensures effective treatment.
Tooth decay isn't just about your teeth; it can affect your whole body. It causes-
- Inflammation and Infection:
- Gum Disease (Periodontitis)
- Cardiovascular Risks
- Respiratory Issues
- Diabetes Impact
- Joint Problems
- Pregnancy Complications
- Chronic Stress
The treatment options for a rotten tooth depend on the severity of the decay. Here are common approaches:
For minor decay, dentists often use dental fillings to restore the tooth's structure. The decayed portion is removed, and the cavity is filled with materials like amalgam or composite resin.
If the decay is extensive, a dental crown may be recommended. This involves capping the tooth with a custom-made restoration, restoring its shape, strength, and appearance.
When decay reaches the tooth's pulp (innermost part), a root canal may be performed. This involves removing the infected pulp, cleaning the canal, and sealing it to prevent further infection.
In severe cases where the tooth cannot be saved, extraction may be necessary. Dentists will explore replacement options, such as dental implants or bridges.
In some cases of infection, antibiotics may be prescribed to eliminate bacteria and prevent the spread of infection.
Always consult with a dentist to determine the most suitable treatment based on your specific condition. Regular dental checkups can help catch decay early, preventing the need for extensive treatments.
The consequences of a rotten tooth can go beyond dental discomfort, affecting your overall health. Here are some potential consequences:
A rotten tooth provides a breeding ground for bacteria. This can lead to a tooth infection, causing pain, swelling, and potential complications if not addressed promptly.
If a tooth infection is left untreated, it can spread to surrounding tissues, jawbone, or even enter the bloodstream. This may result in a systemic infection, impacting other parts of the body.
A pocket of pus (abscess) can develop around the infected tooth. Abscesses can cause severe pain and swelling and pose a risk of spreading infection.
Rotten teeth contribute to gum disease, leading to inflammation, bleeding gums, and potential tooth loss. Gum disease is also linked to systemic health issues like heart disease and diabetes.
Chronic dental infections can weaken the immune system, making it harder for your body to fend off other infections and illnesses.
Untreated dental issues, including rotten teeth, can lead to chronic pain, affecting your daily life and overall well-being.
Difficulty chewing due to dental problems may affect your diet, leading to poor nutrition. This can have broader health implications.
It's crucial to address dental issues promptly to prevent these consequences. Regular dental checkups, good oral hygiene, and seeking timely treatment for dental problems contribute to overall health and well-being.
The question, "Can a rotten tooth make you sick?" reveals a critical connection between oral and systemic health. It's more than a charming smile; it's about safeguarding your overall well-being. Prioritize dental health for a healthier, more vibrant life.
For personalized guidance on maintaining optimal oral health and avoiding risks associated with tooth decay, consult with our dental experts at Springhill Dental Center, AL, who are dedicated to addressing queries related to "Can a rotten tooth make you sick?"
Contact us online or call us at (251) 265-7808 for New Patients and (251) 343-1521 for other callers.
Yes, untreated cavities may contribute to systemic health problems. Timely dental care is essential to address these concerns proactively.
Regular brushing, flossing, and a balanced diet significantly contribute to preventing tooth decay. Incorporate these habits into your daily routine for optimal oral health.
Wondering, "When can I eat solid food after tooth extraction?" Tooth extraction is a simple dental procedure, and though your dentist offers post-operative instructions, the lingering question is about resuming solid foods.
Let's explore to make sure you have the information about "When can I eat solid food after tooth extraction?" and "What to avoid after tooth extraction."
Your mouth needs time to heal after tooth extraction. Consuming solid foods too soon can disrupt the healing process, dislodge the blood clot that forms in the extraction site, and lead to complications like dry sockets. To facilitate proper healing, it's crucial to adhere to the recommended dietary guidelines during the initial recovery period.
Eating solid foods too early after tooth extraction poses several risks. These include increased pain, delayed healing, a higher chance of infection, and the potential for damage to the extraction site. Following your dentist's guidelines ensures a smoother and quicker recovery.
During the initial day's post-tooth extraction, opt for a soft-food diet. This includes:
While focusing on soft foods, it's equally essential to avoid certain types of foods that hinder the healing process. Steer clear of:
The timing varies for each individual, but a general guideline is to wait at least a week before reintroducing solid foods. However, it's crucial to pay attention to your body and only progress to solids when you feel ready. If you experience pain or discomfort, stick to softer options until you're more comfortable chewing.
Most dentists recommend avoiding solid foods for the first 24 hours after tooth extraction. After this initial period, gradually introduce softer solids before transitioning to a regular diet.
It is important to choose the right food after your tooth extraction to heal the extraction site. There are several nutrients that actually help in healing.

When reintroducing solids, prioritize easily chewable and digestible options. Examples include:
Certain nutrients play a crucial role in the healing process. Including foods rich in zinc, vitamins C and A, and protein can promote faster recovery. Consider adding:
To make your post-extraction journey smoother, consider these recommended soft foods:
While it's advisable to avoid chewing on the side of the extraction site, if you can comfortably chew on the opposite side without causing discomfort, it's generally acceptable. However, always follow your dentist's guidance.
If you experience pain while eating, consider taking any prescribed pain medications before your meal. Opt for softer food options and chew slowly to minimize discomfort.
The key to a successful recovery after tooth extraction lies in giving your mouth the time it needs to heal. While the temptation for solid foods may arise, patience is crucial for avoiding complications. Gradually reintroduce solid options, listen to your body, and prioritize soft, nutritious foods to support healing.
For more personalized guidance on “When can I eat solid food after tooth extraction?” and your post-tooth extraction diet, consult our dentist, Dr. Byron Scott, at Springhill Dental Center, AL. You can Contact us online or call us at (251) 265-7808 for New Patients and (251) 343-1521 for other callers.
Remember, a well-thought-out diet contributes significantly to a smooth recovery.
It's advisable to avoid crunchy foods initially to prevent any disruption to the healing process. Stick to softer options.
Yes, some discomfort is normal. If the pain still remains or worsens, consult your dentist.
Gradually reintroduce normal foods as your comfort level allows. Follow your dentist's recommendations.
It's best to stick to lukewarm or cold beverages during the initial recovery period to avoid irritation.
Foods that are rich in vitamins and minerals, such as fruits and vegetables, support the healing process.
Dental care has come a long way, and one of the remarkable innovations in this field is the use of porcelain crowns. If you're considering this dental procedure, you likely have a question, "How long Do Porcelain Crowns Last?" especially in different areas of the mouth.
In this comprehensive guide, we'll explore the functions, durability, and how long do porcelain crowns last based on their placement in the mouth.

Porcelain crowns are versatile dental restorations that play a crucial role in modern dentistry. They are crafted from porcelain, a ceramic material known for its durability and ability to look like natural teeth. It restores both its functionality and aesthetic appeal.
Porcelain crowns, often referred to as dental caps, serve several essential functions in dentistry:
These crowns restore the shape, size, and strength of a damaged tooth. Whether a tooth is cracked, chipped, or weakened by decay, a porcelain crown provides a protective and pleasing solution.
Porcelain crowns act as shields for weakened or decayed teeth. They cover the entire tooth, preventing further damage and maintaining the tooth's structural integrity.
Beyond functional restoration, porcelain crowns contribute to the overall aesthetics of your smile. These are crafted to copy the natural color and shape of your teeth to enhance the appearance of your smile.
When it comes to durability among dental crowns, porcelain crowns stand out as a reliable choice. Their strength and resilience make them a preferred option for long-term dental solutions.

The longevity of porcelain crowns depends on various factors, and understanding these factors is crucial for making informed decisions about your dental health.
High-quality porcelain significantly influences the lifespan of crowns. Crowns made from top-notch materials can last anywhere from 5 to 15 years and, in some cases, even longer.
Consistent and thorough oral hygiene practices play a pivotal role in extending the lifespan of porcelain crowns. Regular brushing, flossing, and routine dental check-ups contribute to the overall health of your teeth and crowns.
Excessive force on your teeth can impact the longevity of your dental crowns. Adopting habits to address these issues can significantly contribute to the durability of your crowns.
The location of the crown in your mouth can influence its lifespan. Crowns in the back of the mouth endure more pressure during chewing, which might necessitate replacement sooner than those in less demanding areas.
In the comparison between porcelain and metal crowns, porcelain takes the lead in terms of durability. Porcelain crowns can withstand wear and tear effectively while maintaining a natural appearance, making them a popular choice.
To enhance the durability of porcelain crowns, consider adopting the following practices:
Maintain an oral care routine to prevent decay around the crown. Regular brushing and flossing, along with professional dental cleanings, contribute to the longevity of your crowns.
If teeth grinding is a concern, using a mouthguard can safeguard both your natural teeth and your crowns. This protective measure helps mitigate the impact of excessive force on your dental work.
You must pay utmost attention to any signs of discomfort, visible damage, or gum issues. Regular dental check-ups can catch potential issues early and allow for timely intervention and adjustments.
Porcelain crowns emerge not just as an investment in dental health but as a blend of functional restoration and cosmetic enhancement. Taking proactive steps in maintaining oral health involves understanding the factors influencing crown lifespan.
Be it on front teeth or molars, porcelain crowns promise lasting benefits with appropriate care. Prioritizing oral hygiene, addressing detrimental habits, and consulting a dentist promptly for arising issues unlock the full potential of porcelain crowns.
At Springhill Dental Health Center, AL, our mission is to craft beautiful and healthy smiles. Whether due for a check-up or contemplating a transformative dental procedure, our experienced team stands ready to support you. Contact us online for appointments or dial (251) 343-1521, and new patients can call (251) 265-7808 for the first step toward a brighter, more confident smile.
Porcelain crowns on front teeth often surpass expectations due to their less demanding role in biting and chewing, potentially exceeding the average lifespan with proper care.
Molars, responsible for grinding and breaking down food, endure more pressure. Porcelain crowns on molars may have a slightly shorter lifespan, underscoring the importance of vigilant oral care.
Research has proven that missing teeth can have a negative impact on your overall health and well-being. However, dental implants have revolutionized the field of dentistry, providing a durable, natural-looking solution for those who are missing one or more teeth.
Dr. Byron Scott at Springhill Dental Center in Mobile, Alabama specializes in dental implants and other restoration options.
While the success rate of dental implants is high, there are situations in which implants must be removed. In this article, we’ll explore the question: can dental implants be removed?

Dental implants are artificial tooth roots made of a biocompatible material, usually titanium, that are surgically implanted into the jawbone. Over time, the jawbone heals around and fuses with the implant through a process known as osseointegration. This creates a stable foundation for the attachment of artificial teeth. The success of the procedure depends on the body’s acceptance of the implant as a natural part of the oral structure.

While dental implants are designed to be a durable and long-lasting solution for tooth replacement, there are instances where removal becomes necessary. Several factors can contribute to the need for dental implant removal, and understanding these common reasons is essential for both patients and dental professionals.
Here are some common reasons dental implants may need to be removed:
Successful dental implants rely on successful osseointegration. If this process does not occur as expected, the implant may not be stable and may need to be removed. In some cases, peri-implantitis may occur. This condition is similar to gum disease and, if left untreated, can lead to jawbone loss and implant failure.
While dental implants are strong and durable, there is a slight risk of fracture. This can be due to excessive force, trauma, or manufacturing defects. A fractured implant may need to be removed to avoid further complications.
While dental implants will not develop decay, they are still susceptible to the effects of gum disease. If not properly maintained, gum disease can lead to inflammation, infection, and the need for removal.
Over time, without stimulation from tooth roots, the jawbone may deteriorate. Dental implants require adequate jawbone density for support, and, without it, the stability of the implants can be compromised.
In some cases, the prosthesis can fail due to mechanical issues, improper fit, or wear and tear.
While titanium is biocompatible, there are other trace metals used in these implants. This can trigger an allergic reaction in some patients, which can lead to implant failure.
Physical trauma to the face/jaw can impact the stability of dental implants. In cases of severe trauma, the implant and surrounding structures may be damaged, which means the implant may need to be removed for the patient’s overall health and well-being.
Certain medical conditions can impact the success of the dental implants. Patients with issues such as uncontrolled diabetes, compromised immune systems, or an autoimmune disorder may experience healing issues and an increased risk of infection.
Improperly placed implants can lead to functional and aesthetic issues. In these cases, removal and re-evaluation may be necessary to achieve optimal results.
The most common challenges of dental implant removal include:
Strong integration of the implant with the surrounding bone makes removal more challenging.
Dental implant removal requires a surgical approach, and in some cases, more invasive techniques may be necessary.
Proximity to nerves and blood vessels poses a risk of damage during removal, leading to potential complications.
Implants may fracture during removal, especially if they have weakened over time or if excessive force is applied.
Minimizing bone loss during removal is crucial for future implant placement or alternative prosthetic solutions.
Dental implant removal is a surgical procedure, and patients may experience discomfort during and after the process.
There is a risk of infection during and after implant removal, particularly if pre-existing issues like peri-implantitis are present.
Preserving the integrity of prosthetic components attached to the implant is important during the removal process.
Complications such as delayed healing or excessive swelling may occur after dental implant removal.
Planning for future restoration, which may involve bone grafting or alternative prosthetic solutions, is essential after implant removal.
Dental implant removal involves specialized techniques to address the challenges associated with the strong integration of the implant with the surrounding bone. The choice of technique depends on factors such as osseointegration, implant stability, and the overall condition of the implant.
The most common techniques Dr. Scott uses for implant removal include:
Manual extraction is suitable when the implant can be manually dislodged. This technique is similar to a tooth extraction. Hand instruments and forceps are used to detach the implant from the surrounding bone.
A surgical approach may be required when osseointegration is strong and more precision is required to minimize damage to the bone. This involves a surgical procedure using rotary instruments or ultrasonic devices to section the implant into removable fragments.
Once the dental implant has been successfully removed, careful attention must be given to post-op care and rehabilitation of the affected area. Depending on the extent of jawbone loss during the procedure, bone grafting may be required to restore the natural contours of the jaw. Additionally, ridge augmentation may be required to prepare the site for future implant placement or alternative restorations.
Dental implants have transformed the landscape of restorative dentistry, providing patients with a reliable, aesthetically pleasing solution for missing teeth. While this restoration has a high long-term success rate, there are risks.
Dr. Scott at Springhill Dental Center in Mobile, Alabama can help you navigate and mitigate these risks, improving your results with dental implants.
Dr. Byron C. Scott and the team at Springhill Dental Health Center are committed to providing comprehensive dental care to the citizens of Mobile, AL and the surrounding areas. We offer a variety of denture options designed to cater to the diverse needs of our patients.
Dentures are a popular, effective solution for individuals dealing with tooth loss. This solution restores functionality, as well as improves the appearance of the smile. In this article, we will explain the types of dentures and cost.

Dentures are removable dental appliances designed to replace missing teeth and surrounding tissues. They serve as a prosthetic solution for individuals who have experienced tooth loss. Dentures play a crucial role in restoring the functionality of the mouth, improving the ability to chew and speak, and enhancing the aesthetic appearance of the smile.
The decision to get dentures is typically based on a combination of factors, and it often involves the assessment and recommendation of a dentist or prosthodontist. Here are some common signs and indicators that may suggest you need dentures:
Persistent toothaches or discomfort, especially if accompanied by gum pain or swelling, may indicate advanced dental issues. If the damage is extensive and cannot be effectively treated with other dental procedures, dentures might be considered.
If you have lost a significant number of teeth, dentures may be a suitable solution. Dentures can replace multiple missing teeth, either in a specific area (partial dentures) or for the entire upper or lower arch (complete dentures).
Problems with chewing or speaking can arise when teeth are missing or severely damaged. Dentures can restore the ability to chew a variety of foods and improve speech, making communication more comfortable and effective.
Gum disease (periodontal disease) can lead to the loss of teeth. If your gums are swollen, red, bleeding, or receding, it may be an indication of gum disease. In cases where the disease has progressed significantly, tooth extraction and dentures may be recommended.
Loose or shifting teeth can be a sign of underlying dental problems. If the supporting structures of the teeth, such as the bone and ligaments, are compromised, dentures may be necessary to restore oral function.
Missing teeth can affect the appearance of your smile and face. If you are dissatisfied with the way your smile looks due to tooth loss, dentures can provide a cosmetic improvement, enhancing your overall facial aesthetics.
Chronic bad breath, also known as halitosis, can be a sign of oral health issues, including advanced tooth decay or gum disease. If these issues are not effectively addressed, tooth loss may occur, leading to the consideration of dentures.
In some cases, the condition of the teeth and gums may be so compromised that other dental treatments, such as crowns, bridges, or dental implants, may not be viable options. Dentures could then become a more suitable and practical solution.

There are several different types of dentures that you need to be aware of if you are considering tooth replacement:
Complete dentures are a full set of artificial teeth designed to replace all natural teeth in either the upper or lower jaw. These dentures are removable and rest on the gums, providing a natural appearance and functional bite. Complete dentures are typically recommended when a patient has lost all of their teeth due to factors such as decay, gum disease, or trauma.
Partial dentures are crafted to replace one or more missing teeth while preserving the remaining natural teeth. These dentures consist of artificial teeth attached to a metal or plastic framework, which is custom-fitted to the patient's mouth. Partial dentures offer both aesthetic and functional benefits, preventing the shifting of remaining teeth and maintaining proper oral alignment.
Immediate dentures are pre-fabricated dentures that are inserted immediately after the removal of natural teeth. These dentures provide immediate tooth replacement, allowing patients to avoid the embarrassment of being without teeth during the healing period. While convenient, immediate dentures may require adjustments as the gums and jawbone heal and change shape.
Implant-supported dentures is a tooth replacement system in which the prosthesis is attached to dental implants. This type of denture offers superior retention, preventing slippage or discomfort associated with traditional dentures. Although implant-supported dentures may have a higher initial cost, many patients find the long-term benefits well worth the investment.

The cost of dentures at Springhill Dental Health Center varies based on factors such as the type of denture, materials used, and additional services required. It's important for patients to understand the different cost components associated with obtaining dentures.
On average, complete dentures can range from $500 to $2,500 per arch. Factors such as the quality of materials, customization, and additional services, like adjustments and follow-up appointments, may contribute to the overall cost.
Partial dentures generally have a lower cost than complete dentures, with prices ranging from $300 to $2,000. The cost is determined by factors such as the number of missing teeth, the materials used in the construction, and the intricacy of the design.
Immediate dentures may have a similar cost range as complete dentures, typically between $500 and $2,500 per arch. Additional expenses may be incurred for adjustments and follow-up appointments to ensure a proper fit as the mouth heals.
Implant-supported dentures represent a higher initial investment due to the surgical placement of dental implants. The cost for implant-supported dentures at Springhill Dental Health Center can range from $1,500 to $4,000 per implant, and a full set of implant-supported dentures may require multiple implants for optimal support.
Springhill Dental Health Center in Mobile, AL, is dedicated to offering a diverse range of denture options tailored to individual patient needs. Whether it's complete dentures, partial dentures, immediate dentures, or implant-supported dentures, the dental professionals at Springhill Dental Health Center prioritize delivering high-quality, personalized solutions.
Understanding the types of dentures and associated costs is crucial for patients seeking tooth replacement options. The team at Springhill Dental Health Center is committed to transparency in pricing and strives to work with patients to find the most suitable and cost-effective solutions for their oral health needs. With a focus on patient satisfaction and oral well-being, Springhill Dental Health Center continues to be a trusted resource for comprehensive dental care in Mobile, AL.
Dental implants have had a significant impact on the world of tooth replacement. They are a reliable, long-lasting solution for those who are missing one or more teeth. While this option has a very high success rate, there is a slight risk of complications. One of the most common complications is gum recession.
Dr. Byron Scott at Springhill Dental Health Center in Mobile, AL, specializes in implant placement and will work with you to ensure the best possible outcome. In this article, we’ll explain more about how to avoid gum recession when getting Dental Implants. We’ll also explore the most common causes of gum recession and some prevention tips.

Gum recession, often referred to as gingival recession, is a process in which the gum tissue pulls away from the tooth or dental implant, which exposes the tooth root or the implant post. There are several factors that can cause or contribute to gum recession, including:
The primary cause of gum recession is poor oral hygiene habits. Failure to practice proper oral hygiene habits leads to the accumulation of bacteria, plaque, and tartar. This causes gum irritation and, ultimately, recession. If dental implants are placed in patients with poor oral hygiene, the risk of complications including gum recession increases.
Many patients believe that it's best to use a firm-bristled toothbrush and aggressive brushing to keep teeth clean. However, when you brush aggressively or with a firm-bristled toothbrush, you may cause damage to the gum tissues, which can cause or worsen gum recession. Instead, use a soft-bristled toothbrush and gentle brushing techniques.
In some cases, gum recession is congenital. Patients with a family history of gum recession are more likely to experience it themselves.
The positioning of the dental implant plays a major role in gum health. If the implant is not placed properly or is too close to the surface, the risk of gum recession increases.
The health and density of the jawbone can impact the stability and appearance of dental implants. If there is not enough bone support, it can lead to gum recession and, ultimately, implant failure.
There are a few things that you can do to prevent gum recession when getting dental implants, including:
While some general dentists and oral surgeons can perform dental implant surgery, it's best to work with a skilled implantologist. These dental professionals are specifically trained in the proper placement and care/maintenance of dental implants. A skilled professional will take the time to assess your personal situation to ensure that the placement of your implants has a low risk of gum recession.
Proper oral hygiene is critical at all times, especially before, during, and after dental implant placement. Proper brushing and flossing as well as regular dental check-ups can reduce the risk of gum disease and gum recession.
A soft-bristled toothbrush and proper brushing techniques can reduce the risk of gum recession and damage to the implants. If you’re not sure what to do, ask your dentist or hygienist for tips on proper brushing.
Regular dental visits- at least every 6 months- are critical for your oral health. These visits allow the dentist to examine your mouth to check for any signs of problems. Early detection is the best way to prevent gum recession.
If you have a personal or family history of gum disease and/or gum recession, it’s a good idea to consult with a periodontist. They will be able to create a custom treatment plan to improve and maintain the health of your gums and dental implants.
If your jawbone doesn’t have the density to support dental implants, bone augmentation can strengthen it and reduce the risk of gum recession.
Smoking significantly increases a patient’s risk of gum recession. Smoking cessation can improve oral and overall health and reduce the risk of oral health complications including gum recession and implant failure.
A skilled implantologist will ensure that the dental implants are properly placed, which creates a natural appearance and reduces the risk of complications.
If gum recession is a concern- or has already started- soft tissue grafts can restore and protect gum tissue.
The best way to avoid issues is to be aware of the potential risks/complications. Discuss these with your implantologist for tips on how to mitigate risks.
Dental implants are an ideal solution for tooth loss. However, while this treatment does have a high success rate, complications may occur. One of the most common complications is gum recession. However, there are steps that you can take to mitigate this risk and improve your chances of a successful experience. Dr. Scott at Springhill Dental Health Center can help you through your implant experience.
If you are among the millions of American adults who are missing one or more teeth, you may be wondering what your options for replacement are. Dr. Byron Scott at Springhill Dental Health Center in Mobile offers several options. One of the most popular ones is dental implants because they are so similar to natural teeth.
Dental implants are surgically inserted into the jawbone, creating a stable base for your prosthetic tooth. This tooth replacement option has been successfully used for more than 3 decades and every year, more than 5 million implants are placed.
Since implants are inserted into the jawbone, they look, feel, and function more like your natural teeth than removable options. However, in order to improve your chances of a successful procedure, it’s important that you:
In this article, we’ll explain what you need to know about dental implants.

A dental implant has three pieces an implant screw, an abutment, and a prosthetic tooth/crown.
Prior to the procedure, Dr. Scott will perform a full examination. This will include reviewing your oral and overall health history, lifestyle habits, and more to determine if you are a good candidate for dental implants. If you are, you can move forward with treatment.
Typically, implants are placed under local anesthesia- but sedation is available for patients who need it. There are different levels of sedation based on your needs. The process typically takes several months to a year to complete. Here’s what you can expect:
If you have remaining natural teeth that must be extracted or active gum disease, this will need to be taken care of prior to implant placement. If you have some jawbone deterioration, a bone graft may be necessary.
Dr. Scott will administer the appropriate anesthesia to help you relax. An incision will be made in the gum and a hole drilled in the jawbone. The implant screw will be placed, and the incision will be closed. In the case of same-day implants or All-on-4, the prosthesis will be placed before you leave the office. If you are getting traditional implants, you will be sent home to heal- which can take up to 6 months.
Once the jawbone has secured the implant screw in place, the incision will be opened, and the abutment will be placed. A healing cap will be placed on this to prevent the gum from healing over it. Impressions will be taken at this time to order your prosthesis or crown.
Finally, your permanent crown will be attached, and your procedure will be complete.
The surgery to place the implants usually takes several hours- especially if multiple implants are required. Therefore, this may not be the ideal option for patients who are at an increased risk of infection.
Dental implants offer several advantages over conventional dentures, including a natural ability to speak and eat. Additionally, there are no special considerations for care and maintenance, you can care for implants like natural teeth.
Research has proven that dental implants are a safe, effective tooth replacement option for most patients. However, this is not the ideal option for everyone. There are a few reasons that may disqualify you from treatment:
If you are missing one or more teeth, Dr. Scott will work with you to determine the best course of treatment.
 Millions of American adults are missing most or all of their natural teeth, which can cause a variety of oral and overall health issues. Therefore, replacement is necessary. Many people choose conventional dentures due to the cost. However, dental implants are the most like natural teeth- unfortunately, the cost is often a barrier.
Millions of American adults are missing most or all of their natural teeth, which can cause a variety of oral and overall health issues. Therefore, replacement is necessary. Many people choose conventional dentures due to the cost. However, dental implants are the most like natural teeth- unfortunately, the cost is often a barrier.
All-on-4 dental implants is a hybrid tooth replacement procedure that blends the stability of dental implants with the affordability of dentures. This procedure replaces an entire arch of missing teeth with 4 strategically placed dental implants. The placement of the implants allows for a much stronger bite force than conventional dentures. Dr. Byron Scott at Springhill Dental Health Center is the top dentist for dental implant placement in Mobile, Alabama.
In this article, we’ll explore more about All-on-4 dental implants.
The implant screw is embedded in your jawbone. The connector attaches the crown to the implant screw, creating a tight seal against your gums. Food should never get stuck between the gum and the implant crown. If this happens, there’s a high probability that the implant was improperly placed. While dental implants have a high success rate, improper placement can ultimately lead to dental implant failure.
The All-on-4 dental implants system offers a variety of benefits, making them one of the best options:
There are very few things that are more uncomfortable than getting food stuck under your dentures. If you have conventional dentures or a removable implant-supported tooth replacement solution, you can simply remove them and clean the food out. However, if you have All-on-4 and food gets stuck underneath them, it can be a bit more challenging.
If the implants and prosthesis are placed properly, you should not have to be concerned about food getting caught. However, there are two reasons why food may get stuck under your All-on-4 dental implants.
If food gets stuck in your dental implants, you’ll have some redness and sensitivity. If not removed quickly, you’re at an increased risk of gum disease and/or infection. Brushing and flossing can help to loosen and remove food debris stuck in dental implants. If food has gotten under the All-on-4 denture arch, you’ll need to contact the clinic for an emergency appointment.
The design of the prosthetic is the most difficult thing to accomplish with All-on-4. It must be designed in such a way that floss can pass underneath/around each implant to remove food debris but create a tight enough seal that food cannot get trapped underneath.
If there is a gap between the prosthetic and your gums, some material can be added to fill in the space.
An acrylic prosthetic is typically the easiest to fix. The prosthetic is simply removed, and additional acrylic is added to build it up and create a better fit. However, if the prosthetic is made from porcelain or zirconia, it’s a bit more challenging. The prosthesis must be removed and adjusted/relined, which can be achieved by filing it down some or by adding porcelain to fill in the gap.
If there are no gaps/spaces between the prosthesis and your gums, the problem may be the shape of the prosthetic. If the prosthesis is made from acrylic, this problem can be solved with a filing instrument. However, if your prosthesis is made from porcelain or zirconia, it is much more difficult to make this type of adjustment. This is because these materials are stronger than acrylic and are susceptible to micro-fractures, which can weaken the prosthesis.
These adjustments can usually be done in the office and only takes a few hours, which means you don’t have to worry about being without your teeth. However, in some situations, major adjustments or repairs must be made, which means the prosthetic will need to be sent to the dental lab.